The emergence and rapid worldwide spread of SARS-CoV-2 have underscored the need for a quick response to biological threats in our current globalized society. Early detection, social distancing, and basic hygiene measures have proven to be of paramount importance to mitigate the viral spread. However, a deeper understanding of the mechanistic underpinnings of new biological threats to human health is crucial. Scientific research helps effectively work towards palliative, curative, and preventive treatment options. Recent studies of COVID-19 have demonstrated that repertoire sequencing of both the T- and B-cell compartments provides essential insights required to understand the pathogenesis, which can, in turn, drive the development of novel therapies and vaccines. In this blog post, we explore how repertoire sequencing advances research and development in the field of infectious diseases and give our view on the future of immunomics-driven therapy development.
Understanding the disease through the immune response
As of writing this post, over 15 million COVID-19 cases have been reported worldwide with over half a million deaths. Clinical symptoms vary from asymptomatic to very severe, many cases of which require mechanical ventilation. The disease severity varies considerably between age groups, with the elderly population and people with underlying medical conditions at a higher severity risk. Researchers across the world have been trying to unravel what factors contribute to this. In a study by Liao et al., single-cell T-cell receptor sequencing of bronchoalveolar lavage fluid showed enrichment of potentially SARS-CoV-2-specific clonally-expanded CD8+ T cells in patients with moderate infections. The clones had upregulated expression of genes related to tissue-residency and showed higher phenotypic variability in severe cases compared to mild and moderate cases [1]. These characteristics advance our understanding of the pathogenesis and could eventually serve as prognostic markers and enable more informed treatment decisions.
The presence of a large and diverse population of clonotypes before pathogen exposure greatly increases the chance of warding off an attack. Sette et al. discuss the finding that a significant proportion of individuals unexposed to SARS-CoV-2 have pre-existing T-cell clonotypes capable of recognizing the pathogen [3]. Potentially, epitope overlap between SARS-CoV-2 and “common cold” coronaviruses are contributing to their higher prevalence. An intriguing possibility is that the information on whether protective B or T cell populations are present in any given individual could be detectable long before initial exposure to the pathogen.
Vaccine development
Vaccination constitutes the best line of defense against life-threatening diseases. A protective immunization not only prevents infection in the vaccinated individual but, if administered to most of the population, also prevents widespread infection and protects immunosuppressed individuals through “herd immunity”. Amidst the current global pandemic, the importance of vaccines is underscored as the means to stop global transmission, with countries around the world in a medical arms race to develop a safe and protective vaccine [4, 5].
Vaccines generate protection by engaging the adaptive immune system to produce a memory compartment of B and T cells that will recognize a pathogen-specific antigen upon re-exposure and eliminate it. The immune receptors are the drivers of specificity, and thus studying their sequence informs of the response elicited to immunization as well as to natural infection. Preliminary studies in SARS-CoV-2 have found highly polyclonal responses with a notable degree of convergence and overlap to previous coronaviruses [6, 7]. The large polyclonality and low affinity maturation observed in these studies seem to indicate that a response that clears the disease might not require a multitude of boosts and should be inducible in most individuals with a non-compromised immune system. Moreover, immune responses in patients clearing the response compared to those that do not can help set a threshold (e.g., affinity maturation, clonal expansion) to test vaccine candidates against.
It is well established that antibodies are the main mechanism of protection in most currently approved vaccines [8]. In concert, T cells play a critical role; cytotoxic CD8+ T cells clear infected cells, and CD4+ T cells are required to provide stimulation to B cells to generate strong antibody responses against protein antigens [9]. Traditional vaccine studies use serological tests to determine immunogenicity and protection, but those tests lack the level of detail needed to inform further immunogen design. High-throughput sequencing allows for in-depth interrogation of large numbers of receptor sequences in parallel, enabling the study of both repertoire-wide properties, such as diversity and clonal expansion, while at the same time supplying the sequences for each receptor involved. Furthermore, by combining high-throughput repertoire sequencing with isolation of monoclonal antibodies, the specificity and affinity of individual receptors can be overlaid onto the whole repertoire [10]. The development of methods to leverage repertoire sequencing data for vaccine studies can shorten development time and help in the global fight against emerging biological threats.

Antibody development
Therapeutic monoclonal antibodies are the go-to treatment option for many afflictions because of their high specificity and extended half-life compared to other drugs. Their development makes use of the immune system’s ability to generate thousands of novel potential drug candidates. In the case of a global pandemic, exploiting naturally occurring antibodies can accelerate the development of treatments to help combat the spread and mitigate the severity and decrease hospitalization time. Thus, parallel to the quest for a protective vaccine, there is an ongoing effort to obtain monoclonal antibodies that prevent SARS-CoV-2 infection utilizing high-throughput sequencing technologies [11, 12].
The common methodologies to produce monoclonal antibodies are screening display libraries or hybridoma-based workflows post immunization. In both approaches, the methodology’s limitations reside in the capacity to analyze at most a few hundred antibodies for phenotypical properties like affinity to the antigen. High-throughput sequencing of immune repertoires brings a wealth of data, which allows analyses such as tracking clones over time, finding clonal overlap, and building phylogenetic trees to find and prioritize the most promising candidates for expression and phenotypical analysis. Moreover, this technology allows to virtually find any clonal relative of a well-performing antibody with better affinity for the antigen, longer half-life, or fewer sequence liabilities.
Infected individuals produce large amounts of antibodies to combat a disease. If these repertoires can be interrogated at sufficient depth, that can lead to the discovery of monoclonal antibodies that can be used for treatment. For example, studies of HIV-1 infected individuals have uncovered a myriad of neutralizing antibodies that are being clinically tested to treat infected individuals [13]. High-throughput repertoire sequencing opens the possibility to leverage the high number of infected and recovered individuals in a pandemic to find best-in-class neutralizing antibodies to use as therapeutics.
The future of immunomics-driven R&D in infectious disease
Recently, community-spawned, open-access immune receptor databases have seen a significant rise in contributions. These databases contain an unprecedented amount of (paired) receptor sequences, often including information on their antigen-specificity, with, for example, the VDJdb offering over 20.000 paired T-cell receptor sequences, as of writing [14]. These receptor datasets aid efforts to develop methods for in silico prediction of antigen specificity using machine learning strategies. For instance, researchers at the University of Antwerp have developed TCRex, a tool that predicts TCR epitope binding for human T-cell receptors, with prediction models for over 50 different epitopes. They also offer a tool that enables researchers to train models based on their own datasets [15].
Here at ENPICOM, we have developed a specialized software solution to help identify and extract commonly occurring receptors from patient cohorts. For instance, by comparing the antibody repertoires of patients that have recovered from COVID-19, you can identify and quantify common, disease-specific antibody sequences that are the result of convergent recombination. These antibodies can be used as a starting point for drug development or help identify ‘high-activity’ serum samples to treat COVID-19 patients effectively.
The synergy between ever-expanding public databases and innovative computational approaches could lead to the development of antigen-agnostic prediction models and enable truly de novo inference of receptor antigen specificity. This could usher in a revolution in healthcare, where immune fingerprints are built from a single blood draw, potentially enabling disease detection before emergence of symptoms and improving the accuracy of prognoses. These two factors can determine the need and type of therapeutic intervention, as well as the expected clinical benefit, which is crucial for truly personalized treatment decisions.
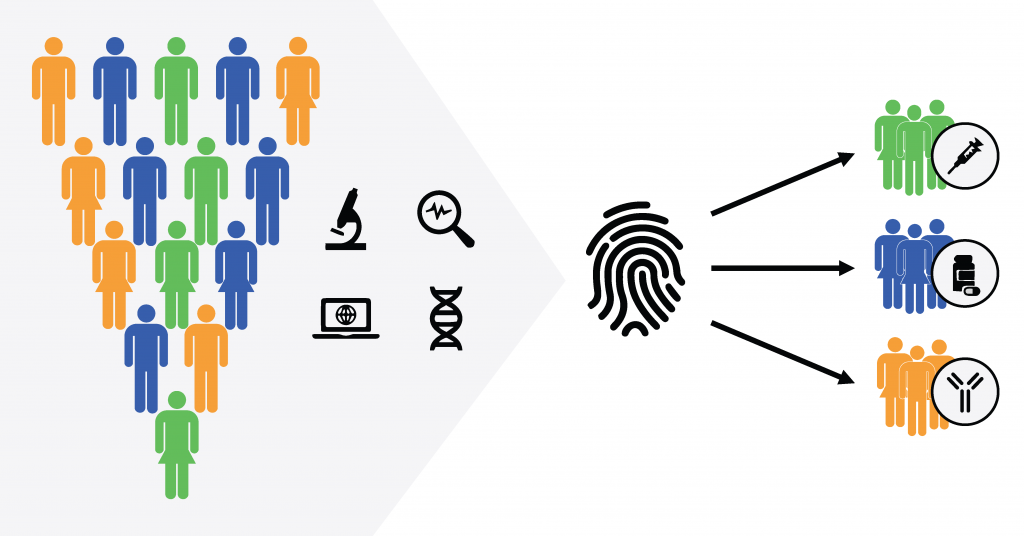
Immune fingerprinting could revolutionize the way we approach health care.
Continually increasing affordability and throughput of sequencing technologies are synergizing with a myriad of novel computational methods. This could soon bring de novo inference of receptor antigen specificity within reach. These developments should pave the way for a revolution in healthcare, enabling early detection and bringing novel approaches to rational development of vaccines and other therapeutics. Given the scale and severity of the devastating sociological and economic impact of the current pandemic, the need for innovative tools to understand emerging infectious diseases and rapidly develop biomarkers and therapeutics is clearer than ever.
Bibliography
[1] M. Liao et al., “Single-cell landscape of bronchoalveolar immune cells in patients with COVID-19,” Nature Medicine, 2020.
[2] L. Gutierrez et al., “Deciphering the TCR Repertoire to Solve the COVID-19 Mystery,” Trends in Pharmacological Sciences, 2020.
[3] A. Sette et al., “Pre-existing immunity to SARS-CoV-2: the knowns and unknowns,” Nature Reviews Immunology, 2020.
[4] P. Folegatti et al., “Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a preliminary report of a phase 1/2, single-blind, randomised controlled trial,” The Lancet, 2020.
[5] F.-C. Zhu et al., “Immunogenicity and safety of a recombinant adenovirus type-5-vectored COVID-19 vaccine in healthy adults aged 18 years or older: a randomised, double-blind, placebo-controlled, phase 2 trial,” The Lancet, 2020.
[6] S. C. A. Nielsen et al., “Human B cell clonal expansion and convergent antibody responses to SARS2 CoV-2,” bioRxiv, 2020.
[7] J. D. Galson et al., “Deep sequencing of B cell receptor repertoires from COVID-19 patients reveals strong convergent immune signatures,” bioRxiv, 2020.
[8] S. A. Plotkin et al., “Correlates of protection induced by vaccination,” Clinical and vaccine immunology, 2010.
[9] S. L. Nutt et al., “The generation of antibody-secreting plasma cells,” Nature Reviews Immunology, 2015.
[10] G. E. Phad et al., “Extensive dissemination and intraclonal maturation of HIV Env vaccine-induced B cell responses,” Journal of Experimental Medicine, 2019.
[11] W. B. Alsoussi et al., “A Potently Neutralizing Antibody Protects Mice against SARS-CoV-2 Infection,” Journal of Immunology, 2020.
[12] L. Hanke et al., “An alpaca nanobody neutralizes SARS-CoV-2 by blocking receptor interaction,” bioRxiv, 2020.
[13] C. Possas et al, “HIV cure: global overview of bNAbs’ patents and related scientific publications,” Journal Expert Opinion on Therapeutic Patents, 2018.
[14] D. Chudakov et al., “VDJdb,” [Online]. Available: https://vdjdb.cdr3.net/. [Accessed 14.07.2020].
[15] S. Gielis et al., “TCRex: a web tool for the prediction of TCR–epitope recognition,” [Online]. Available: https://tcrex.biodatamining.be/. [Accessed 15.07.2020].